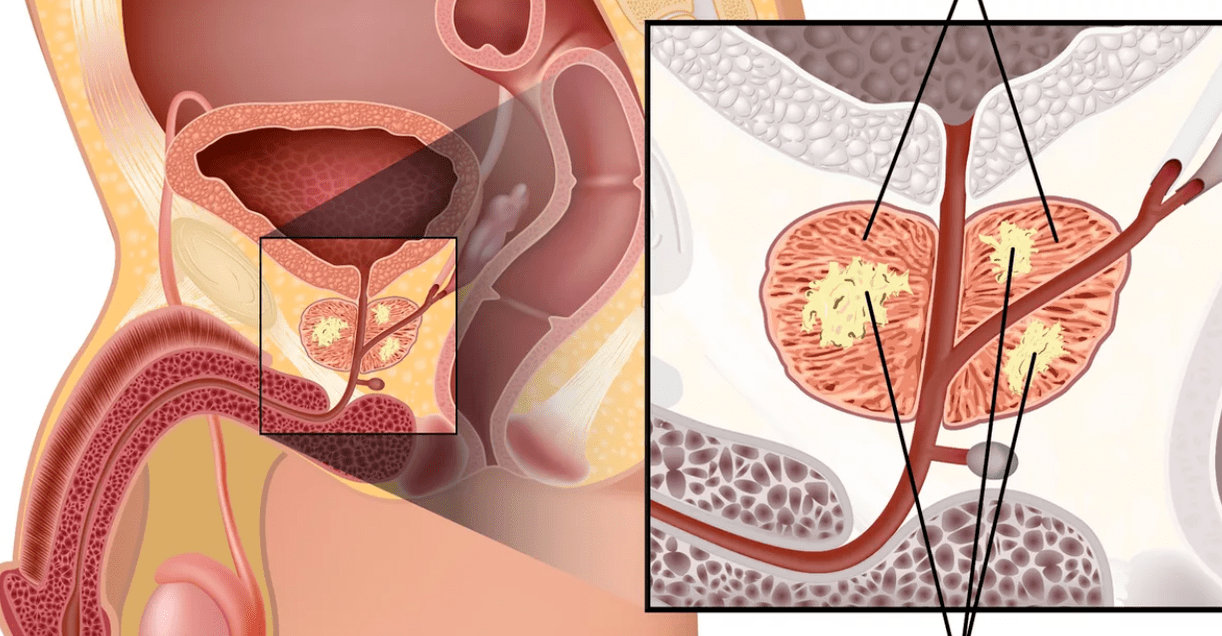
Calculous prostatitis- aggravation of chronic inflammation of the prostate gland, characterized by the formation of stones in the gland's acini or excretory ducts. Calculous prostatitis is accompanied by increased urination, dull aching pains in the lower abdomen and perineum, erectile dysfunction, blood in the seminal fluid, and prostatorrhea. Calculous prostatitis can be diagnosed using digital examination of the prostate, ultrasound of the prostate gland, questionnaire urography and laboratory examination. Conservative therapy for calculous prostatitis is carried out with the help of drugs, herbal medicines and physiotherapy; If these measures are ineffective, destruction of the stone with a low-intensity laser or surgical removal is indicated.
General Information
Calculous prostatitis is a form of chronic prostatitis, accompanied by the formation of stones (prostatoliths). Calculous prostatitis is the most common complication of the long-term inflammatory process in the prostate gland, which specialists in the field of urology and andrology deal with. Stones in the prostate gland are detected in 8. 4 percent of men of different ages during preventive ultrasound examination. The first age peak of the incidence of calculous prostatitis occurs at 30-39 years of age and is associated with an increase in cases of chronic prostatitis caused by STDs (chlamydia, trichomonosis, gonorrhea, ureaplasmosis, mycoplasmosis, etc. ). Calculous prostatitis in 40-59-year-old men, as a rule, develops against the background of prostate adenoma, and in patients over 60 years of age, it is associated with a decrease in sexual function.
Causes of calculous prostatitis
Depending on the cause of formation, prostate stones can be true (primary) or false (secondary). Primary stones initially form directly in the acini and ducts of the gland, while secondary stones pass from the upper urinary tract (kidneys, bladder or urethra) to the prostate if the patient has urolithiasis.
The development of calculous prostatitis occurs as a result of congestive and inflammatory changes in the prostate gland. BPH, irregular or lack of sexual activity, and sedentary lifestyle are the causes of prostatic discharge disorder. Against this background, the addition of a slow infection of the genitourinary tract leads to blockage of the prostate ducts and a change in the nature of the prostate secretion. In turn, prostate stones also support the chronic inflammatory process and stagnation of secretions in the prostate.
In addition to stagnation and inflammation, urethro-prostatic reflux, pathological reflux of a small amount of urine from the urethra to the prostate ducts during urination - plays an important role in the development of calculus prostatitis. At the same time, the salts in the urine crystallize, thicken and turn into stones over time. The causes of urethro-prostatic reflux are narrowing of the urethra, injury to the urethra, atony of the prostate gland and seminal tubercle, previous transurethral resection of the prostate gland, etc. can be.
The morphological core of prostate stones is amyloid bodies and desquamated epithelium, which gradually "grew" with phosphate and lime salts. In the prostate gland, stones are located in cystically swollen acini (lobules) or excretory ducts. Prostatoliths are yellowish in color, spherical in shape, different in size (on average 2. 5-4 mm); can be single or multiple. Prostate stones are chemically similar to bladder stones. Most oxalate, phosphate and urate stones are formed with calculous prostatitis.
Symptoms of calculous prostatitis
Clinical manifestations of calculous prostatitis are generally similar to the course of chronic inflammation of the prostate. The leading symptom in the clinic of calculous prostatitis is pain. The pain is dull, aching in nature; localized on the perineum, scrotum, pubis, sacrum or coccyx. Exacerbation of painful attacks may be associated with defecation, sexual intercourse, physical activity, prolonged sitting on a hard surface, prolonged walking, or bumpy driving. Calculous prostatitis is often accompanied by urinary incontinence, sometimes complete retention of urine; hematuria, prostatorrhea (leakage of prostate secretion), hemospermia. It is characterized by decreased libido, weak erection, ejaculation disorder and painful ejaculation.
Endogenous prostate stones can remain in the prostate gland for a long time without symptoms. However, a long course of chronic inflammation and associated calculous prostatitis can lead to the formation of prostate abscess, development of vesiculitis, atrophy and sclerosis of glandular tissue.
Diagnosis of calculous prostatitis
To make a diagnosis of calculous prostatitis, consultation with a urologist (andrologist), assessment of existing complaints, physical and instrumental examination of the patient is required. When performing a rectal digital examination of the prostate, a lumpy surface of stones and a kind of crepitus are determined by palpation. Using transrectal ultrasound of the prostate gland, stones are detected as hyperechoic formations with a clear acoustic trace; their location, quantity, size and structure are clarified. Sometimes, examination urography, CT and MRI of the prostate are used to detect prostatoliths. Exogenous stones are diagnosed by pyelography, cystography and urethrography.
Instrumental examination of a patient with calculous prostatitis is completed with laboratory diagnostics: examination of prostate secretion, bacteriological culture of urethral discharge and urine, PCR examination of scraps for sexually transmitted infections, biochemical analysis of blood and urine, determination of the level of prostate gland-specific antigen, biochemistry of sperm, ejaculationculture etc.
During examination, calculous prostatitis is differentiated from prostate adenoma, tuberculosis and prostate cancer, chronic bacterial and bacterial prostatitis. In calculous prostatitis not associated with prostate adenoma, prostate volume and PSA level remain normal.
Treatment of calculous prostatitis
Uncomplicated stones with chronic inflammation of the prostate gland require conservative anti-inflammatory therapy. Treatment of calculous prostatitis includes antibiotic therapy, non-steroidal anti-inflammatory drugs, herbal medicines, physiotherapeutic procedures (magnetic therapy, ultrasound therapy, electrophoresis). In recent years, low-intensity lasers have been successfully used to destroy prostate stones non-invasively. Prostate massage is strictly contraindicated for patients with calculous prostatitis.
Surgical treatment of calculous prostatitis is usually required when the disease is complicated, combined with prostate adenoma. When an abscess of the prostate gland is formed, the abscess is opened and the passage of stones is noted along with the discharge of pus. Sometimes mobile exogenous stones can be instrumentally pushed into the bladder and subjected to lithotripsy. Removal of large fixed stones is performed in the process of perineal or suprapubic division. When calculous prostatitis is combined with BPH, the optimal surgical treatment method is adenomectomy, TUR of the prostate, prostatectomy.
Prognosis and prevention of calculous prostatitis
In most cases, the prognosis for conservative and surgical treatment of calculous prostatitis is favorable. Long-term non-healing urinary fistulas can be a complication of perineal removal of prostate stones. If left untreated, calculous prostatitis results in prostate abscess and sclerosis, urinary incontinence, impotence, and male infertility.
The most effective measure to prevent stone formation in the prostate gland is to contact a specialist at the first signs of prostatitis. An important role is related to the prevention of STIs, elimination of predisposing factors (urethro-prostatic reflux, metabolic disorders), age-appropriate physical and sexual activity. Preventive visits to a urologist and timely treatment of urolithiasis will help prevent the development of stone prostatitis.






























